
Risk Stratification Overview
Benefits of Risk Stratified Population Health Management
Risk Stratification Model Example [Pyramid]
Risk Stratification for High-Risk Patients
Incorporating Risk Stratification Into Diabetes Care Workflow
Successful Risk Stratification for Diabetes
Risk Stratification Overview [Definition & Caveats]
In most healthcare organizations, individuals are classified as low-risk, rising-risk, high-risk, and highly complex, wherein the highly complex group requires the most resources and intensive care. “Risk” refers to the likelihood of an adverse clinical outcome, such as a worsening of symptoms, declining quality of life due to illness or injury, or death.
For example:
- An otherwise healthy individual who catches the common cold needs a short office visit and no referrals. This patient would be classified as low-risk.
- An individual with a BMI of 30, a history of substance abuse, and out-of-range biometrics makes frequent visits to their primary care clinician for related health issues, but has not yet developed any chronic conditions. This patient would be considered rising-risk.
- An individual with Type 2 diabetes and multiple comorbidities requires extra pre-visit planning, longer in-office appointments with their clinician, referrals to specialists or home care providers, and an extended follow-up plan. This patient would be classified as high-risk or highly complex.
With a combination of objective data and subjective insights, health systems use algorithms to determine where and how to allocate resources, identify which patients to prioritize, and predict how patients’ needs will change due to their condition or other precipitating medical factors. Patients are then placed within a risk stratification model designed to inform clinical care decisions.
While this process provides health systems with a more complete view of their patient population, the traditional approach to risk stratification is less clinically effective — and less cost-effective — than intended. Dividing patients into distinct, homogeneous subgroups risks ignoring the nuanced needs of individuals in the highly complex category. This is especially true for patients with multiple chronic, complex conditions like diabetes, who incur astronomical healthcare costs over their lifetime but do not require the same type of care as a patient with late-stage cancer.
By transforming the way their practices operate and categorize patient needs, clinicians and care teams gain a more accurate view of their patient populations, resulting in more holistic and personalized treatment plans.
Benefits of Risk Stratified Population Health Management
In order to effectively manage their patient population, clinical practices must consider patients as both individuals and members of a larger population group By classifying patients into distinct subgroups based on their conditions, medical needs, and level of risk, practices can:
- Select patients who would benefit from working with a specialist
- Identify patients for coordinated care solutions
- Improve scheduling (i.e. schedule longer appointments for higher-risk patients)
- Prioritize existing resources and identify needs gaps
However, the resulting distinct subgroups do not account for patients who may fall between two categories of risk, and therefore may not receive optimal care or the most appropriate resources for their condition. This is particularly important for smaller clinical practices that may lack the resources to effectively serve the full spectrum of rising-risk, high-risk, and highly complex populations.
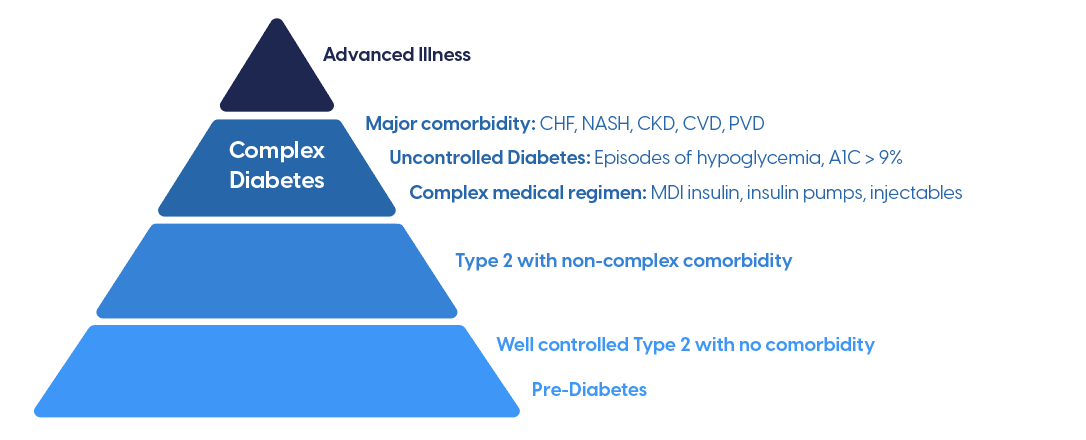
Risk Stratification Model Example [Pyramid]
Patient risk levels are typically displayed using a pyramid diagram, with the patients with the most complex (and therefore, expensive) needs placed at the apex. The practical purpose of this structure is to prioritize the patients with the highest level of risk, then allocate resources accordingly for each level.
Defining High Need Patients with Complex Diabetes
This model, while effective for organizing patients at a high level, is not entirely accurate when more factors are taken into consideration. Patients may fall into distinct categories based on their objective medical needs, but risk missing out on critical care because their clinician’s risk stratification model does not account for social determinants of health. The inability to afford medications, lack of health insurance, or lack of a support system at home can negatively impact an otherwise low-risk patient, causing their risk level to rise.
Risk Stratification for High-Risk Patients
High-risk patients with chronic illnesses account for 90% of the nation’s $3.8 trillion in annual healthcare spending. The individuals in the highly complex category alone, which represent only 5% of the U.S. patient population, account for half of that sum.
In 2020, clinical researchers at Kaiser Permanente made two important discoveries when they analyzed the electronic health record (EHR) data of the system’s 4 million patients. First, they found that the top 5% of high-risk patients were much more diverse than previously thought. These individuals could be classified into three distinct groups:
- People with one or more chronic medical conditions that can be improved or kept under control
- People who had suffered a one-time catastrophic health problem
- People with severe chronic conditions who can’t be returned to good health and require expensive, continuous treatment
Second, the researchers found that the people in the first two categories change unpredictably from year to year. Their discoveries make a case for reassessing value-based care models that target the top 5% of patients, which are not designed to accommodate this diversity and unpredictability.
Using this information, the researchers proposed a new model for treating patients with chronic illnesses by focusing on both “those who are currently in the top 5% and those who could end up there in the coming years if their medical problems worsen and their health deteriorates.” Clinical practices may see a reduction in the number of patients who fall into the critically ill top 5% by incorporating the following elements into their workflow:
Integrate disease management programs with ongoing primary care
Programs dedicated to addressing one disease often interact with patients independently of their clinicians. Virtual disease-management services are convenient for patients, but keeping clinical and virtual care in silos creates more work and drives costs up for patients, clinicians, and insurance payers. To avoid the fragmentation of a patient’s care — or the duplication of a clinician’s work — these programs need to involve the entire clinical care team.
Utilize clinical support staff
With only a year of formal training, medical assistants and other clinical support staff can assume multiple responsibilities from primary care clinicians. These team members — who earn roughly half of a nurse practitioner’s salary — can review patient information, extract and assemble data for the clinician, provide the patient with educational resources, and coordinate lab or specialist services. This support enables a clinician to devote more time to see their patients.
Leverage technology
Telehealth enables patients to access care and clinical guidance, even if they can’t make it to the office. Using a combination of phone calls, video calls, secure messaging, photos, and digital healthcare tools, a clinician or nurse practitioner can just as easily assess a patient’s needs as if they were in the exam room. For example, nurses or medical assistants can perform a visual assessment of a patient via smartphone video, potentially identifying areas of concern weeks before a patient can schedule an in-person appointment.
Enable pharmacists to make medication adjustments
In many states, pharmacists can be licensed to adjust medication dosages as needed using protocols established by clinicians. This affords clinicians even more time to see high-need patients.
Incorporating Risk Stratification Into Diabetes Care Workflow
A traditional patient risk taxonomy classifies patients based on medical factors like comorbidities; however, a more accurate model would account for a patient’s social determinants of health, including their level of engagement, socio-economic status, age, health history, lifestyle, access to healthcare and related resources, and social support network.
According to Dr. James Dom Dera, writing for Family Practice Management, there are several ways to implement risk stratification into clinical practice workflow depending on patient population, staff, and available resources:
- Use a daily team huddle to discuss and assign risk levels to the patients who are scheduled to be seen that day or the next.
- Focus on a specific patient population, such as patients with diabetes, and assign an office staff member to run a report showing all of your patients sorted by A1C level. For each patient with an A1C over 9, delegate a clinical team member to assign a final risk level after further consideration of subjective data.
- Use designated weekly or monthly team meetings to discuss and assign risk levels to all patients, beginning with those whose objective data suggest they are at potentially highest risk.
In categorizing patients with diabetes, the lines of the traditional risk stratification model are not always sufficient or accurate. A patient may have an A1C above 9, but have strong family or social support at home. Therefore, they may be assigned a lower risk level than a patient with an A1C of 9.6, no social support, and an inability to adhere to treatment recommendations. This example demonstrates the need for risk stratification to be a dynamic process that allows for reassessment and individualized, contextual adjustments.
Successful Risk Stratification for Diabetes
The goal of managing high-risk and highly complex patients is to keep costs down while providing the most comprehensive, coordinated care solutions available. To deliver the right care to the right patients at the right time, risk stratification models need to account for non-medical patient characteristics including:
- Mental and behavioral health
- Income level
- Access to healthcare and community services
- Social and familial support
- Ability to adhere to treatment programs and disease self-management
Accounting for these characteristics can help practices leverage lower-cost care management services that prevent avoidable health emergencies or the need for acute services.
By taking an updated approach to risk stratification, value-based practices and health systems can connect patients with high-risk, complex diabetes to:
- Care management programs that provide one-on-one support for medical and social needs
- Coaches or care advocates who work with patients to ensure they receive appropriate education, care services, medication recommendations, and scheduling assistance
Using proprietary technology and a team of clinical diabetes experts, the Stability Health model of care provides comprehensive support to patients with complex diabetes, including those who may be mis-categorized based on objective data or those who may fall between risk levels.
Each Stability Health participant receives a dedicated health coach who serves as a liaison between the patient, their clinician, and a team of Stability Health clinical experts. Due to the direct connection forged between health system clinicians and the Stability Health care team, coaches can identify potential risks long before a patient’s next appointment. Coordination with each patient’s clinician enables Stability Health to alert clinicians of changes in a patient’s health status or life circumstances, ensuring the patient is classified and prioritized appropriately within their primary care practice.
Timely interventions like this are crucial in keeping healthcare costs down, preventing avoidable health emergencies, and improving the lives of patients with complex — but entirely manageable — diabetes.



